Many experts believe that chronic prostatitis is an inflammatory disease caused by infection and may be accompanied by autoimmune diseases, which is characterized by damage to the parenchyma and interstitial tissues of the organs. This disease has been known medically since 1850, but even today, it is still poorly understood and the response to treatment is poor. Chronic bacterial (6-10%) and non-bacterial (80-90%) prostatitis are the most common and socially significant inflammatory diseases in men, significantly reducing their quality of life. The disease is mainly seen in young and middle-aged people, and is often accompanied by impaired mating and reproductive functions (decreased potency, infertility, etc. ). The disease is documented in 8-35% of male cases between 20 and 40 years old.
The cause of bacterial prostatitis is the purulent flora, which invades the glands from the urethra or through lymph and blood. The etiology and pathogenesis of chronic non-bacterial prostatitis are still unclear. It mainly affects men over 50 years of age.
Causes of disease development
Chronic prostatitis is currently considered a political disease. There is a view that the disease is caused by infection invading the prostate, and then the pathological process proceeds without its involvement. Many non-infectious factors contribute to this.
Infectious factors in the development of chronic prostatitis
In 90% of cases, the pathogen enters the gland from the urethra, causing acute or chronic prostatitis. There have been cases of asymptomatic carriers. The course of the disease is affected by the body's defense status and the biological characteristics of the pathogen. It is speculated that the transition from acute prostatitis to chronic prostatitis is due to the excessive production of fibrous tissue resulting in loss of tissue elasticity.
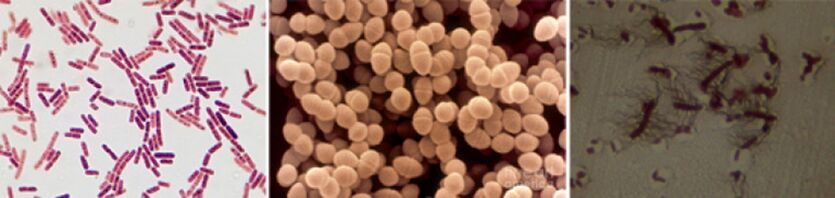
Among the pathogens of chronic prostatitis, the following pathogens were found:
- In 90% of cases, the disease will show Gram-negative bacteria, such as E. coli, Enterococcus faecalis (Enterococcus faecalis), but less common-Pseudomonas aeruginosa, KlebsiellaBacteria, Proteus, Pseudomonas aeruginosa and Enterobacter. Gram-positive bacteria Enterococcus, Streptococcus and Staphylococcus are rare.
- The role of coagulase-negative Staphylococcus, Ureaplasma, Chlamydia, Trichomonas, Gardnerella, anaerobes and Candida fungi has not been fully elucidated.
Infection enters the prostate in several ways:
- The frequent combination of prostatitis and urethritis proved the most likely ascending path.
- Hematogenous prostatitis occurs when the infection penetrates into the glands with the bloodstream, and is seen in chronic tonsillitis, sinusitis, periodontitis, pneumonia, cholecystitis and cholangitis, and purulent skin diseases.
- Through contact, chronic prostatitis can develop into urethritis and urethral stricture. When the infection enters the glands with the flow of urine, it is accompanied by purulent infection of the kidneys. During the diagnosis and treatment of urology, it can cause epididymitis through the tubule route. , Vas deferens and ropeway inflammation (catheterization, urethral insertion), including transurethral.
- Lymphatic infections penetrate the prostate through proctitis, hemorrhoidal vein thrombophlebitis, etc.
Non-infectious factors in the development of chronic prostatitis
Chemical factors
According to experts, the leading role in the development of chronic prostatitis is urine reflux in the prostate. When urine enters the glands from the urethra, the emptying of the prostate and seminal vesicles is impaired.
With the development of the disease, the vascular response develops, leading to organ edema, the nervous and humoral regulation of the urethral smooth muscle tissue tension is disturbed, and the activation of αOne-Adrenergic receptors lead to the development of dynamic obstruction and lead to the development of new reflux in the prostate.
The urate contained in the urine, with the reflux, leads to the development of a "chemical inflammatory response".
Hemodynamic disorders
They support chronic inflammation and circulatory disturbances of the pelvic organs and scrotum. Traffic jams occur in people with sedentary lifestyles, such as drivers, office workers, etc. , accompanied by obesity, sexual abstinence, sexual disorders, frequent hypothermia, mental and physical overload. Spicy stimulates the intake of food, alcohol and smoking, etc. , which help maintain the inflammatory process.
other factors
There are many other factors that support chronic prostate inflammation. These include:
- Hormones.
- Biochemical.
- The immune response is impaired.
- Autoimmune mechanism.
- Infection and allergy process.
- The characteristics of the prostate gland structure make it difficult to completely drain.
Often, the cause of the development of chronic prostatitis cannot be determined.
Classification of prostatitis
According to the classification proposed by the National Institutes of Health in 1995, prostatitis is divided into:
- Acute (Class I). It is 5-10%.
- Chronic bacteria (Class II). Yes 6-10%.
- Chronic non-bacterial inflammation (Class IIIA). It is 80-90%.
- Chronic non-bacterial non-inflammatory (Class IIIB) or chronic pelvic pain syndrome.
- Chronic prostatitis, accidentally diagnosed (Class IV).
Signs and symptoms of chronic prostatitis
Chronic prostatitis has a long course, but it is not monotonous. The period of relative calm that occurs after complex anti-inflammatory and antibacterial treatments replaces the period of exacerbation.
The development of chronic bacterial prostatitis usually precedes bacterial or gonorrhea urethritis, non-bacterial-circulatory disorders (hemorrhoids, chickenpox, etc. ) of the pelvic organs and scrotum (hemorrhoids, chickenpox, etc. ), excessive sexual behavior.
Patients with chronic prostatitis have many complaints. They have seen a doctor for many years, but rarely check for prostate disease. Approximately one-quarter of patients have no discomfort or have few clinical symptoms when the disease progresses.
The main complaints of patients with chronic prostatitis can be conditionally divided into several groups.
Urinary system diseases related to urethral stricture:
- Difficulty starting to urinate.
- Weak urine flow.
- Urinate intermittently or dropwise.
- Feeling of incomplete bladder emptying.
Symptoms caused by nerve ending irritation:
- Frequent urination.
- The urge to urinate is sharp and violent.
- Urinate in small amounts.
- Urinary incontinence when urinating.
Pain syndrome:
- The intensity and nature of pain are different.
- Pain location: lower abdomen, perineum, rectum, groin and lower back, inner thigh.
Sexual dysfunction:
- The rectum and urethra are painful during ejaculation.
- Slow erection.
- Loss of orgasm.
- Premature ejaculation and so on.
In terms of the nervous system: a neurotic disorder that focuses the patient’s attention on their health.
Signs and symptoms of chronic nonbacterial prostatitis
Male chronic pelvic pain syndrome (CPPS) has the common symptoms of chronic prostatitis, but there are no bacteria in the third part of the urine and the secretions of the prostate. CPPS can simulate chronic non-bacterial interstitial cystitis, rectal disease, spastic pelvic floor myalgia syndrome, and functional prostate disease caused by organ innervation and its hemodynamic disturbances.
If neurovegetative function is impaired, weakness and invasion of glandular innervation will occur, and it is difficult to quickly and completely close the urethral cavity. At the same time, the urine after urination will continue to be excreted drop by drop for a long time. In these patients, studies have shown increased instability and excitability, which is manifested by increased sweating and increased excitability of cardiac activity, as well as dermatological changes.

Complications of the disease
The long-term course of chronic prostatitis is complicated by impaired sexual and reproductive functions, the development of diseases such as seminal vesiculitis and epididymitis, and organ sclerosis. The sclerosis of the organ will worsen the local microcirculation and urodynamics, as well as the result of surgical intervention. Fibrosis of the tissues around the urethra leads to the development of urinary system diseases.
diagnosis
Since there are many reasons for the development of chronic prostatitis, a series of diagnostic studies are used to diagnose it. The success of treatment depends on correctly determining the cause of the disease. The diagnosis of chronic prostatitis is based on the following data:
- A typical triad.
- A set of physical methods (digital rectal examination of the prostate).
- A set of laboratory methods (urinalysis and microscopic examination of prostate secretions, culture and determination of the susceptibility of the microbiota to antimicrobial drugs, general analysis of urine and blood).
- Bacterioscopy, PCR and serological methods for the detection of Neisseria gonorrhoeae and urethral smears (for the detection of Ureaplasma and Chlamydia).
- Urine fluorescence method.
- Prostate biopsy.
- Complex instrument method (ultrasound).
- Determine the patient's immune status.
- Determine the state of nerves.
- If the treatment is ineffective and complications are suspected, computer and magnetic resonance imaging, blood culture and other tests are performed.
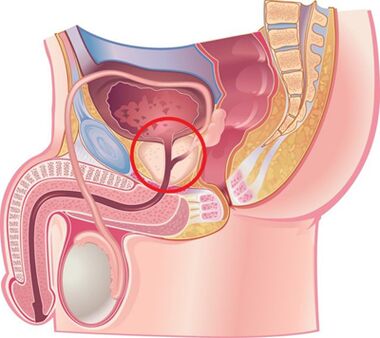
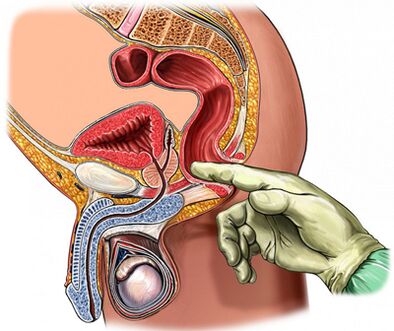
Prostate Palpation
The most important thing in the diagnosis of the disease is the palpation of the prostate. The palpation of the prostate increases during the worsening period, and decreases during the reduction of the inflammatory process. In chronic prostatitis during iron deterioration, edema and pain may occur.
The density of the organ consistency can be different: palpate softened and compacted areas, identify recessed areas. During palpation, the shape of the glands, the condition of the seminal nodules and surrounding tissues can be assessed.
The process of transrectal digital examination is combined with the collection of glandular secretions. Sometimes it is necessary to obtain the secret from each share separately.
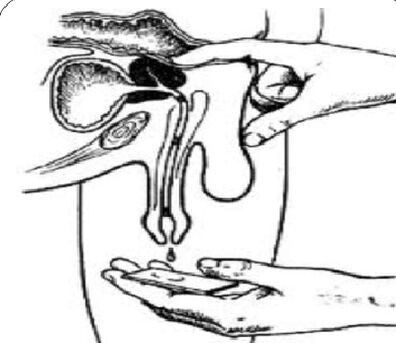
Analysis of 3 cups of urine and prostate secretions
The "gold standard" for the diagnosis of chronic prostatitis is:
- Collect the first part of urine.
- Collect the second part of urine.
- Get the secretions of the glands through massage.
- Collect the third part of urine.
In addition, microscopic and bacteriological examinations were performed on the materials.
With inflammation of the prostate:
- Microbe count (CFU) exceeds 103/Ml (10four/ml for Staphylococcus epidermidis), but don’t ignore dozens and hundreds of microorganisms.
- Through microscopic examination, the presence of 10-15 white blood cells in the field of view is a generally accepted standard for the existence of inflammatory processes.
The secrets of the prostate and the third part of urine are examined by microscope and bacteriology:
- In chronic bacterial prostatitis, the number of white blood cells in glandular secretions increases, and the third part of urine after massage will release bacteria (mainly intestinal flora).
- For non-bacterial prostatitis, the number of white blood cells in glandular secretions increases, but the microbiota is not detected.
- With CPPS, the number of white blood cells and microbiota did not increase.
Normal rate of prostate secretion:
- There are less than 10 white blood cells in the field of view.
- There are many lecithin particles.
- The microflora does not exist.
In chronic prostatitis, the secretions of the prostate show:
- The number of white blood cells is large-more than 10-15 in the field of view.
- The amount of lecithin particles is reduced.
- The pH of secretions tends to be alkaline.
- The content of acid phosphatase is reduced.
- The activity of lysozyme increases.
Once there is no inflammatory process, obtaining a negative result of prostate secretion does not prove.
Retain the value of the prostate secretion crystallization test. Usually, during the crystallization process, a characteristic pattern in the form of fern leaves is formed. If the aggregation properties of prostate secretions are disrupted, this pattern will not form, which happens when the androgen background changes.
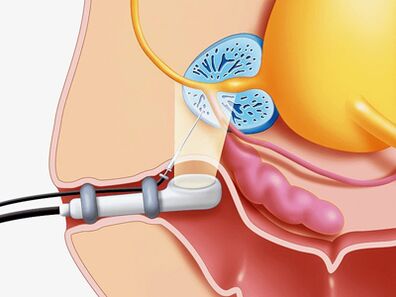
Ultrasound procedure
If prostate disease is suspected, ultrasound examination of the gland itself (transrectal ultrasound is best), kidneys and bladder can be used to determine:
- The volume and size of the gland.
- The presence of stones.
- The size of the seminal vesicles.
- The condition of the bladder wall.
- Residual urine volume.
- Scrotal structure.
- Another type of pathology.
Other ways to check the prostate
- Urodynamic status (a study of urine flow rate) can be easily and simply determined using studies such as uroflow measurement. With the help of this research, the signs of bladder outlet obstruction can be found in time and dynamic observations can be made.
- If abscess formation, benign hyperplasia, and prostate cancer are suspected, a needle biopsy is performed.
- In order to clarify the cause of the obstruction under the bladder, X-ray and endoscopy were performed.
- If there is a long-term inflammatory process, urethral cystoscopy is recommended.
Differential diagnosis
Chronic prostatitis should be related to bladder prostatic hypertrophy, autonomic prostate disease, congestive prostatitis, pelvic floor myalgia, neuropsychiatric disorders, pseudosynergism, reflex sympathetic dystrophy, inflammatory diseases of other organs: interstitialDifferentiation of cystitis, bladder joint osteitis, prostate and bladder cancer, hyperthyroidism, urolithiasis, chronic epididymitis, and inguinal hernia.
Chronic prostatitis treatment
The treatment of chronic prostatitis should start from changing the patient's lifestyle and diet.
In the treatment of diseases, drugs that affect different links of the pathogenesis are used at the same time.
Main treatment direction:
- Eliminate pathogenic microorganisms.
- Anti-inflammatory treatment.
- The blood circulation of the prostate and pelvic organs is normalized.
- The normalization of adequate drainage of the prostate gland.
- Normalization of hormonal profile.
- Prevent organ sclerosis.
For the treatment of chronic prostatitis, the following groups of drugs are used:
- Antibacterial.
- Anticholinergic.
- Vasodilators.
- ΑOne-Adrenergic blockers.
- 5 Alpha reductase inhibitor.
- Cytokine inhibitors.
- Non-steroidal anti-inflammatory drugs.
- Vasoprotective agent.
- Immunomodulator.
- Drugs that affect the metabolism of uric acid.
Antibiotic treatment of chronic bacterial prostatitis
Antibiotic treatment should take into account the sensitivity of the identified microorganisms to antibiotics. If the pathogen is not identified, use empirical antimicrobial therapy.
The preferred drugs are II-IV generation fluoroquinolones. They quickly penetrate into glandular tissues through the usual application methods, and are active against a large group of Gram-negative microorganisms as well as Ureaplasma and Chlamydia. If antimicrobial treatment fails, one should assume:
- The multi-drug resistance of the microbial community,
- Short (less than 4 weeks) treatment course,
- Wrong choice of antibiotics and their doses,
- Changes in pathogen types,
- The bacteria present in the ducts of the prostate are covered by a protective outer cell membrane.
The duration of treatment should be at least 4 weeks, with mandatory follow-up bacteriological control. If there are more than 10 bacteriuria in the third part of urine and prostate secretions3CFU/ml, the course of repeated antibiotic therapy is 2 to 4 weeks.
Cytokine inhibitors for chronic prostatitis
Cytokines are glycoproteins secreted by immune cells and other cells in response to inflammation and immune responses. They actively participate in the development of chronic inflammatory processes.
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs have anti-inflammatory effects and relieve pain and fever. They are widely used in the form of tablets and suppositories to treat chronic prostatitis. The most effective route is rectal administration.
Immunotherapy
In the treatment of bacterial chronic prostatitis, in addition to antibiotics and anti-inflammatory drugs, immunomodulators are also used. The most effective is rectal administration. Immunomodulators are widely used, which increase the functional activity of phagocytes and help eliminate pathogens more effectively.
Alpha-receptor blockers in the treatment of chronic prostatitis
It has been determined that α-1 adrenergic blockers can normalize the smooth muscle tone of the prostatic urethra, seminal vesicles and prostate vesicles, which makes this group of drugs very effective in treating the disease. Alpha-1 adrenergic blockers are used for patients with severe urinary system diseases without active inflammatory processes.
The duration of treatment for CPPS is 1 to 6 months.
5a-reductase inhibitors in the treatment of bacterial prostatitis and CPPS
Studies have found that under the action of 5a-reductase, testosterone is converted into 5a-dihydrotestosterone in the form of the prostate. Its activity in prostate cells is more than 5 times higher than the activity of testosterone itself. It is due to the epithelial and matrix components in the elderly. Causes an increase in organs.
After taking 5a-reductase inhibitor for 3 months, interstitial tissues atrophy, within 6 months-glands, secretory function is suppressed, the severity of pain syndrome and gland volume are reduced, organ tension and edema are alleviated.
The role of anti-sclerosis drugs in the treatment of chronic prostatitis
With prolonged inflammation of the prostate, fibrosis occurs, which is manifested by impaired microcirculation and urodynamics. In order to prevent the fibrotic process, anti-sclerosis drugs are used.
Other drugs used to treat chronic prostatitis
Together with the above drugs, the following drugs are used to treat the disease:
- Antihistamines.
- Vasodilators and vasoprotectants.
- Immunosuppressive agent.
- Drugs that affect the metabolism of uric acid and trisodium citrate.
Herbal products
Prostatitis can be effectively treated using a preparation in the form of a suppository, which contains a complex of biologically active peptides isolated from bovine prostate.
Occurs under the influence of drugs:
- Stimulates metabolic processes in glandular tissues.
- Improve microcirculation.
- Reduce edema, white blood cell infiltration, stagnation of secretion and pain.
- Prevent prostatic venule thrombosis.
- Increase the activity of acinar secretory epithelium.
- Improve sexual function (increase libido, restore erectile function and normalize spermatogenesis).
Prostate finger massage
Many researchers believe that taking into account the known contraindications, finger massage should be used to treat chronic prostatitis.
physiotherapy
The effectiveness of physical therapy procedures in the treatment of prostatitis has not been confirmed today, the mechanism of action has not been scientifically determined, and adverse reactions have not been studied.
Prevent chronic prostatitis
When starting to prevent the development of chronic prostatitis, you should know:
- Over the years, the risk of this disease will increase.
- Representatives of the black race are more likely to get sick.
- The family susceptibility of the disease cannot be ruled out.
People who are prone to chronic prostatitis should pay more attention to their health.
Disease prevention tips:
- Drink more water. Frequent urination promotes the exudation of microbiota from the urethra.
- Prevent diarrhea and constipation.
- Balanced diet. Avoid eating foods rich in carbohydrates and saturated fats, which can lead to weight gain.
- You should limit the use of substances that irritate the urethra as much as possible: spicy foods, bacon, sauces and seasonings, coffee and alcohol.
- Stop smoking. Nicotine adversely affects the condition of blood vessel walls.
- Don't get too cold.
- Do not keep the bladder empty.
- Live an active lifestyle and exercise. Exercise strengthens the pelvic floor muscles, which can eliminate venous congestion, thereby supporting normal prostate function.
- Regular sex life. Avoid long-term abstinence. The gland must be released from the secret quickly.
- Maintain a monogamous relationship. Indiscriminate sex will increase the possibility of contracting sexually transmitted diseases.
- If you have urogenital discomfort, please contact your urologist immediately.

























